Novel Coronavirus, COVID-19 and How to Deal with the Virus in the
Indoor Environment: An Update
Ching-Yi Tsai, Ph.D. and Chin S. Yang, Ph.D.
A lot has happened since our last newsletter
dealing with the disease COVID-19 caused by the
novel coronavirus SARS-CoV-2. This update
provides additional information to help you deal with
the virus.
The Massachusetts Institute of Technology
(MIT) reports that under the right conditions the virus containing droplets and
gas clouds (aerosols) may travel up to 27 feet. These conditions are influenced
by: gravity pull, wind direction and velocity, temperature fluctuations,
relative humidity,
and the duration and intensity of sunlight
(UV). Clearly the greater the distance between individuals and virus containing
droplets or aerosols the less likely the chance of the virus infecting
individuals, thus the importance of SOCIAL DISTANCING to decrease the risk and
to reduce
spread of the virus.
There are more reports and evidences on
asymptomatic or symptomless virus carriers among us.
This strengthens the importance of social
distancing, handwashing and wearing a mask. Handwashing with hot water
(caution: not too hot to burn skin) is even more effective than with
cold water. Using hot water cycle or
adding bleach in your laundry can eradicate any possible viral
particles in the laundry. World Health
Organization (WHO) website reports that SARS-CoV-2 virus
can be inactivated at 56°C (or 133°F) or higher,
although it does not provide additional details, such
as moist heat.
Another issue being hotly debated is the
use of mask by non-essential personnel, non-medical professionals and non
COVID-19 patients. Different grades of masks have different filtration
efficiencies and protection. Respirators
with filter cartridges may offer a very high degree of
protection if users are fit tested. N95
masks offer a very high degree of protection against viral
particles. Surgical masks and cloth masks
may not offer as a high degree of protection as N95. At a
minimum, they create a barrier between our
nasal openings and possibly contaminated air. If you
use a mask, make sure you change it, wash
it and/or disinfect it regularly. Wash your hands with
soapy water before putting on the mask and
after removing the mask. Obviously, we don’t want to
compete with the medical professionals for
their supplies of N95 mask.
If an indoor space, whether it is a
school, an office building, a supermarket, a food store, or a public building,
is suspected to be exposed to a confirmed case or to a COVID-19 patient,
sanitization or disinfection may be necessary. We suggest the followings:
1. Do not do any testing for the virus. It is unlikely you can
find the testing anyway because all
the sampling and testing resources are used for medical purposes.
Sampling and testing may take a few days. If it is contaminated, there is no
time to waste on testing. Go ahead and plan for disinfection.
2. In additional to 60-70% alcohols, hydrogen peroxides, and
diluted solutions of bleach or chlorine-releasing compounds. You can add heat
or hot water at 60 °C (or 140°F) or higher into your arsenal for inactivation
of SARS-CoV-2 virus. Hot water extractors used in carpet shampooing and
cleaning can be used in such situations, provided 60°C hot water is used.
3. Consider using a combination of different disinfectants and
different techniques of application. Fogging with hydrogen peroxides or diluted
bleach solutions plus surface wiping with any of the four disinfectants. We
want to emphasize the incompatibility of bleach solutions with other chemicals,
including peroxides, alcohols, ammonia and ammonia-containing cleaners. So use
them with the greatest caution.
4. Make sure there is sufficient contact time for the
disinfection. In general, a 15 minutes contact is recommended for
disinfections. In our previous newsletter, we suggest less than 15 minutes may
be enough to inactivate SARS-CoV-2 virus, based on a review of SARS literature.
A longer contact time will ensure proper disinfections.
5. Wipe surfaces where people are in frequent contact with diluted
bleach solutions, wait for 15 minutes, then wipe with clean hot water, and
finally dry the surfaces.
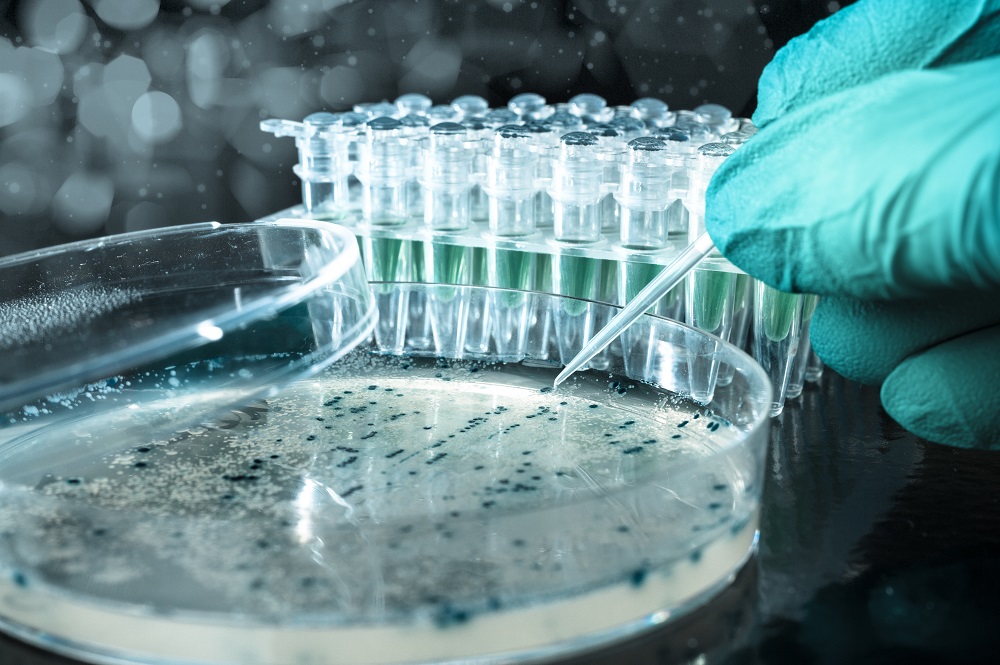
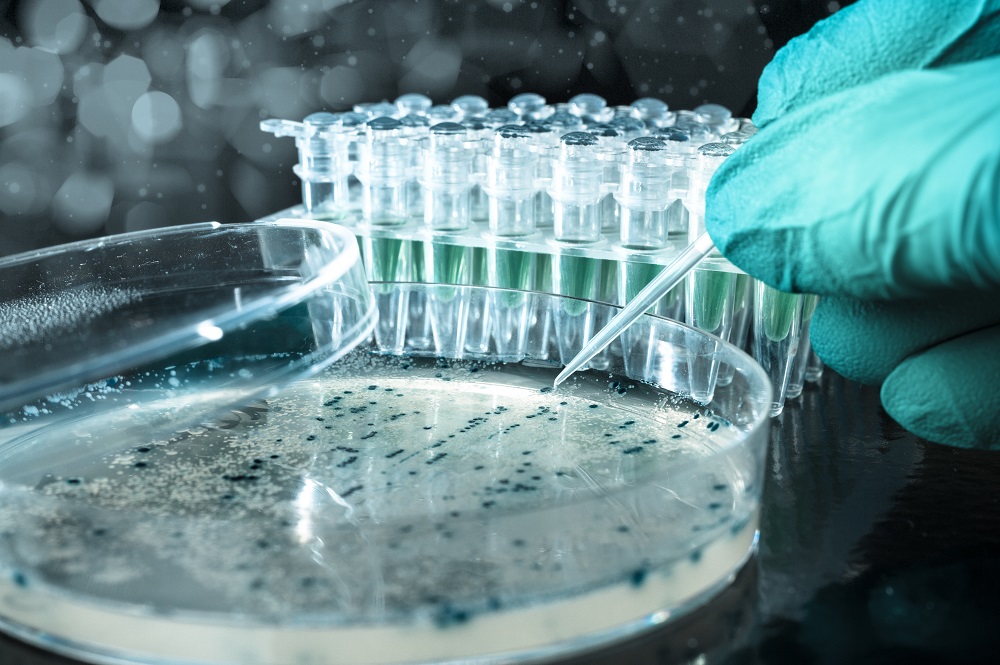
6. Post remediation/disinfection verification (PRV) can be
achieved by taking surface swab samples and test them for bacteria and fungi as
surrogates for the virus . A couple of reference
samples from similar but non-impacted areas should be collected and analyzed
for comparisons. Samples from disinfectant treated areas should have below
detection or greatly reduced (>90% reduction) bacterial and fungal levels.
As always, know your disinfectants. Read
instruction labels on the disinfectant containers or MSDSs, if they are
available, before using them. These disinfectants should only be used and
applied by professionals when used in large scales.
Our senior microbiologist, Dr. Ching-Yi
Tsai, was a member of the Taiwanese team that identified
and completed whole genome sequences of
SARS virus in patients in Taiwan. She helped to determine the replication and
pathogenesis of SARS coronavirus. If you have any questions concerning the new
coronavirus, SARS-CoV-2 or COVID-2019, you can reach her at 856-767- 8300 or
[email protected]. Our effort to develop a RT-PCR method for the
detection of the virus from the environment has been greatly delayed by the
unavailability of some supplies and reagents. We do not believe the supplies
and reagents will be available anytime soon due to government’s efforts to
control the outbreak.
Scientific basics of
SARS-CoV-2
COVID-19 is the pneumonia or disease
caused by SARS-CoV-2 virus. SARS-CoV-2 belongs to a
large family of single-stranded RNA
viruses. RNA is the genetic material of the virus. A structural
diagram of the virus is below for your
reference. Coronaviruses are enveloped with a lipid layer
embedded with structural proteins. They
use its spike glycoprotein (S) to bind its receptor, and
mediate membrane fusion and entry of virus
RNA. Recently, researchers confirmed that SARSCoV-
2 uses human-angiotensin-converting enzyme
2 (hACE2) as the receptor to enter human cells through endocytosis. By
denaturalizing proteins and disrupting its envelope using the disinfectants
discussed above, the virus cannot bind to
the cell receptor and enter the human cells.
References:
Xiuyuuan Ou
and Zhaohui Qian et al. Characterization of spike
glycoprotein of SARS-CoV-2 on virus entry and its immune crossreactivity
with SARS-CoV. Nature. 27 March 2020.
https://www.nature.com/articles/s41467-020-15562-9#Sec13
Marco Cascella, Michael Rajnik, Arturo
Cuomo, Scott Dulebohn and Raffaela
Napoli. Features, Evaluation and Treatment Coronaviruses(COVID-19).
March 2020. https://www.ncbi.nlm.nih.gov/books/NBK554776/
Kampf, G., D. Todt,
S. Pfaender, and E. Steinmann. 2020. Persistence of
coronaviruses on inanimate surfaces and their inactivation with biocidal
agents. Journal of Hospital Infection,
https://doi.org/10.1016/j.jhin.2020.01.022
Ong,
Sean W. X., Yian K Tan, Po Y. Chia, Tau H. Lee, Oon T. Ng, Michelle S. Y. Wong, and Kalisvar
Marimuthu. 2020. Air, Surface Environmental, and
Personal Protective Equipment Contamination by Severe Acute Respiratory
Syndrome Coronavirus 2 (SARS-CoV-2) From a Symptomatic Patient. JAMA. March 4,
2020.
doi:10.1001/jama.2020.3227
Van Doremalen, N., Trenton Bushmaker,
Dylan H. Morri, Myndi G.
Holbrook, Amandine Gamble, Brandi N. Williamson, Azaibi
Tamin, Jennifer L. Harcourt, Natalie J. Thornburg,
Susan I. Gerber, James O. Lloyd-Smith, Emmie de Wit, Vincent J. Munster.
Aerosol and surface stability of HCoV-19 (SARS-CoV-6 2) compared to SARS-CoV-1.
https://doi.org/10.1101/2020.03.09.20033217
Yeh, S.H., H.Y. Wang, C.Y.
Tsai, C.L. Kao, J.Y. Yang, H.W. Liu, I.J. Su, S.F. Tsai, D.S. Chen, P.J.
Chen & National Taiwan University SARS Research Team. Characterization of
SARS coronavirus genomes in Taiwan: Molecular epidemiology and genome
evolution. Proc. Natl. Acad. Sci. USA 101:2542-2547, 2004.
Date:
April 3, 2025